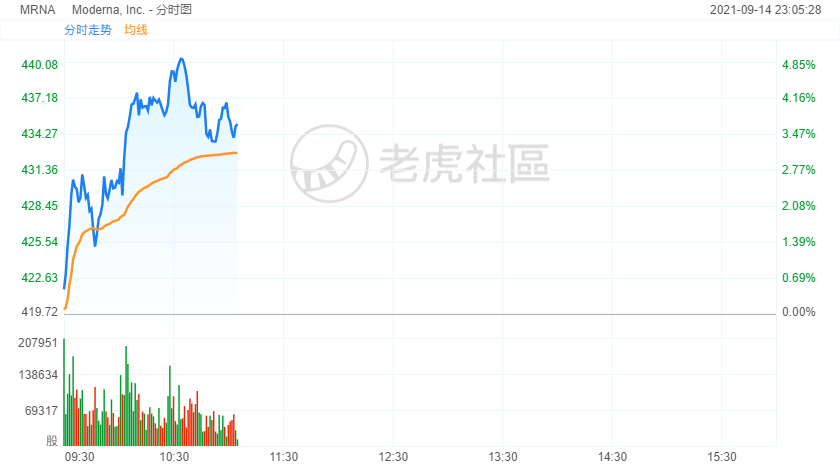
Moderna stock jumped 4% in morning trading as a recent study found that the Moderna COVID-19 vaccine produces higher antibody levels than the Pfizer-BioNTech vaccine.
- A recent study found that the Moderna COVID-19 vaccine produces higher antibody levels than the Pfizer-BioNTech vaccine.
- This is possibly due to its higher mRNA content and a longer waiting period between doses.
- Antibody tests are not entirely predictive of the body’s immunity against COVID-19.
A recent study found that the Moderna COVID-19 vaccine produced twice as many antibodies in recipients as the Pfizer-BioNTech vaccine.
The August study, published in JAMA, compared the antibody levels of 1647 healthcare workers before and six to 10 weeks after vaccination. The researchers observed significantly higher antibody levels among the recipients of the Moderna vaccine compared to the recipients of the Pfizer-BioNTech vaccine.
Among all the participants who had a previous COVID-19 infection, those who were vaccinated with the Moderna vaccine still carried more antibodies.
However, more research is needed to understand whether the difference in antibody levels leads to different levels of protection against the virus. Experts stress that testing for antibodies isn't the only way of measuring protection.
Why Does Moderna Produce Higher Antibody Levels?
According to the authors of the study, the Moderna COVID-19 vaccine contains more mRNA and requires a longer waiting period than Pfizer-BioNTech, which may have played a role.
“It is also possible that the mRNA itself used in the Moderna vaccine may have led to this difference independent of the dose in the vaccine or the timing of the two shots,"Richard Martinello, MD, Yale Medicine infectious diseases specialist and associate professor of medicine and pediatrics at the Yale School of Medicine, who was not involved in the study, tells Verywell.
The Moderna vaccine contains more mRNA within the vaccine compared to the Pfizer dosage. And doses are given 28 days apart, compared to 21 days for the Pfizer vaccine.
Still, further research is needed to understand why Moderna produced more antibodies. Experts still aren't sure if varying antibody levels translate to a difference in protection against COVID-19.
Antibody Tests Don’t Tell the Whole Story
The study has notable limitations since it focused solely on healthcare workers and did not include data on cellular immunity.
“Antibody levels have been found to provide a good measure of one’s protection against infection,” Martinello says. “However, it is known that cellular immunity plays a key role in the protection against and response to COVID. This is much more difficult to measure so it is not a routine test available from clinical laboratories. Therefore, while it is possible that the Moderna vaccine may be found to be more protective than the Pfizer vaccine, that remains to be seen.”
A May study found that antibody levels can be predictive of protection from COVID-19 infection, but the researchers acknowledged that it's important to study T cell and B cell memory responses as well.
Although antibody levels are much simpler and cheaper to measure, and higher levels are likely to be more protective, they’re not a good measure of the degree and/or duration of protection an individual has against COVID-19,Stanley H. Weiss, MD, professor of medicine at the Rutgers New Jersey Medical School and professor of biostatistics at the Rutgers School of Public Health, tells Verywell.
Earlier this year, the Food and Drug Administration (FDA) issued guidance saying that antibody tests should not be used to assess COVID-19 immunity after vaccination.3Researchers say that antibody tests are valuable public health tools that have very little use for individuals, and should not influence personal decision-making.
“There is ample data showing that some persons without any detectable antibodies have good protection due to cellular immunity,” Weiss says. “There is also ample data of breakthrough infection among persons who have anti-Covid antibodies.”
A March study found that cellular immunity remains robust six months after natural infection even though antibodies against the virus may fall below detectable levels. The findings show promise that COVID-19 vaccines elicit a similar response in the body.
“In an individual person for clinical purposes, and especially outside of a carefully designed research study, I recommend against antibody testing,” Weiss says. “Neither a positive nor negative result gives you definitive information. My recommendation is for a decision to be based on general clinical criteria, not on an antibody test.”